
NEW RESEARCH
Are Your Utilization Management Strategies built for what's coming?
How Top Decision makers Are Tackling Their Hardest Challenges
For over a decade, payers have grappled with a trio of barriers: soaring medical costs, complex administrative & regulatory processes, and workforce limitations. These issues span not just logistical, but also technological—as interoperability and real-time-access needs continue to grow.
This exclusive analysis reveals the operational shifts, tech investments, and other strategies payers are prioritizing now. See how your peers are adapting—and where you may be falling behind.
This research, commissioned by Medecision, gathers perspectives from more than 50 C-Suite leaders, offering invaluable insights for those seeking to make a significant impact in the healthcare sector.
A crucial finding is the importance of 'contextual understanding' of the member. By integrating various data sources, health plans can achieve a more comprehensive understanding of individual needs, leading to better health outcomes.
Download The Full Report Today
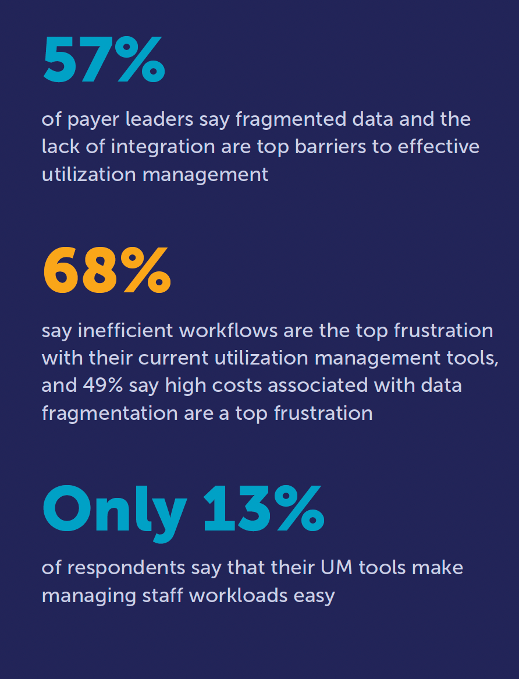
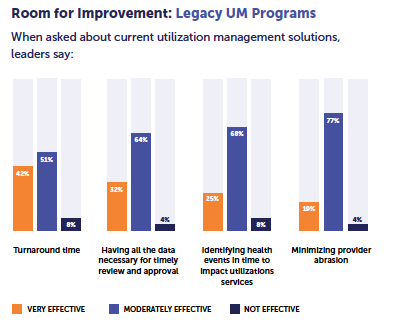
Current legacy tools are hindering the effectiveness of utilization management (UM), care management (CM), and population health management (PHM), leading to a fragmented and frustrating experience. Help your organization drive down costs and improve outcomes with exclusive access to comprehensive insights from top health plan executives about the current state of UM, CM, and PHM as of 2024.
Discover key strategies to break down the barriers impeding progress.